

BOSULIF (bosutinib) tablets
Pfizer
SUPPLEMENTAL INDICATION: Newly-diagnosed chronic phase (CP) Philadelphia chromosome-positive chronic myelogenous leukemia (Ph+ CML).
EFFICACY:
- Open-label, randomized, multicenter trial, n=487 patients with Ph+ newly-diagnosed CP CML, bosutinib 400 mg once daily vs. imatinib 400 mg once daily
- Major efficacy outcome: Major molecular response (MMR) at 12 months, defined as ≤0.1% BCR ABL ratio on international scale (corresponding to ≥3 log reduction from standardized baseline) with a minimum of 3000 ABL transcripts as assessed by the central laboratory.
- 47.2% (95% CI: 40.9, 53.4) vs. 36.9% (95% CI: 30.8, 43.0), p=0.0200
SAFETY:
- Most common adverse reactions: Diarrhea, nausea, thrombocytopenia, rash, increased alanine aminotransferase, abdominal pain, and increased aspartate aminotransferase
REGULATORY PATHWAY: sNDA
- Priority Review, and Orphan Drug designation, Accelerated approval for supplemental application
- Approval based on molecular and cytogenetic response rates; continued approval may be contingent upon verification and confirmation of clinical benefit in an ongoing long-term follow up trial
- First approval in 2012 for treatment of patients with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
REIMBURSEMENT:
- 100% of Medicare Part D and Medicare Advantage plans coverage
- Tier 5 (specialty); Co-pay based on coverage stage
- Patient Assistance programs

GIAPREZA (angiotensin II) injection
La Jolla Pharmaceutical Company
FIRST INDICATION: Increases blood pressure in adults with septic or other distributive shock
ADDRESSING UNMET NEED:
- Shock can result in organ failure and death
- Need for treatment options for critically ill hypotensive patients who do not adequately respond to available therapies
MECHANISM OF ACTION: Angiotensin II raises blood pressure by vasoconstriction and increased aldosterone release
EFFICACY:
- Single double-blind study, n=321 adults with septic or other distributive shock, GIAPREZA vs.placebo
- Primary endpoint: % of subjects with Mean Arterial Pressure (MAP) ≥ 75 mmHg or a ≥ 10 mmHg increase in MAP without an increase in baseline vasopressor therapy at 3 hours
- 70% vs. 23%, p < 0.0001 (treatment effect of 47%)
SAFETY:
- Can cause dangerous blood clots with serious consequences (clots in arteries and veins, including deep venous thrombosis)
- Prophylactic treatment for blood clots should be used
REGULATORY PATHWAY: NDA
- Priority Review
- Required pediatric assessments
REIMBURSEMENT:
- Available March 2018

CABOMETYX (cabozantinib) tablets
Exelixis
SUPPLEMENTAL INDICATION: Treatment of patients with advanced renal cell carcinoma (RCC)
EFFICACY:
- Single, randomized, open-label phase 2 multicenter study, n=157 patients with intermediate and poor-risk previously untreated RCC, Cabometyx vs. sunitinib
- Endpoint: Estimated median progression-free survival (assessed by blinded independent radiology review committee)
- 8.6 months (95% CI: 6.8, 14.0) vs. 5.3 months (95% CI: 3.0, 8.2), p=0.0008
SAFETY:
- Most commonly reported adverse reactions: Diarrhea, fatigue, nausea, decreased appetite, hypertension, palmar-plantar erythrodysesthesia, weight decreased, vomiting, dysgeusia, and stomatitis
- Most frequent grade 3-4 adverse reactions: Hypertension, diarrhea, hyponatremia, hypophosphatemia, PPE, fatigue, ALT increased, decreased appetite, stomatitis, pain, hypotension, and syncope
REGULATORY PATHWAY: sNDA
- Approval provides for treatment in first-line setting
- Previous approval in 2016 for treatment of patients with advanced RCC who have received prior anti-angiogenic therapy
REIMBURSEMENT:
- 100% of Medicare Part D and Medicare Advantage plans coverage
- Tier 5 (specialty); Co-pay based on coverage stage
- Patient Assistance programs
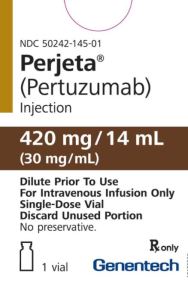
PERJETA (pertuzumab)
Genentech
SUPPLEMENTAL INDICATION: In combination with trastuzumab and docetaxel for the treatment of patients with HER2-positive metastatic breast cancer who have not received prior anti-HER2 therapy or chemotherapy for metastatic disease
EFFICACY:
- Single multicenter, randomized, double-blind, n= 4804 patients with HER2-positive early breast cancer with primary tumor excised prior to randomization, PERJETA vs placebo
- Efficacy outcome: Invasive disease-free survival (IDFS), defined as the time from randomization to first occurrence of ipsilateral local or regional invasive breast cancer recurrence, distant recurrence, contralateral invasive breast cancer, or death from any cause
- Intent to Treat population: 7.1% (n=171) vs. 8.7%, p=0.047
- In patients with hormone receptor negative disease: 8.2% vs. 10.6%
- In patients with node positive disease: 9.2% vs. 12.1%
- Overall survival data are not yet mature
SAFETY:
- Adverse reactions: Diarrhea, nausea, alopecia, fatigue, peripheral neuropathy, and vomiting
- Most common grade 3-4 adverse reactions: Neutropenia, febrile neutropenia, diarrhea, neutrophil count decreased, anemia, white blood cell count decreased, leukopenia, fatigue, nausea, and stomatitis
REGULATORY PATHWAY: sBLA
- Fulfills post-marketing requirement for 2013 accelerated approval
- First approval in 2012 for use in combination with trastuzumab and docetaxel for HER2-positive metastatic breast cancer with no prior therapy
- Accelerated approval in 2013 as neoadjuvant treatment
REIMBURSMENT:
- 70% of Medicare Part D and Medicare Advantage plan coverage
- Tier 5 (specialty); Co-pay based on coverage stage
- Patient Assistance programs
Image credit: DailyMed, La Jolla